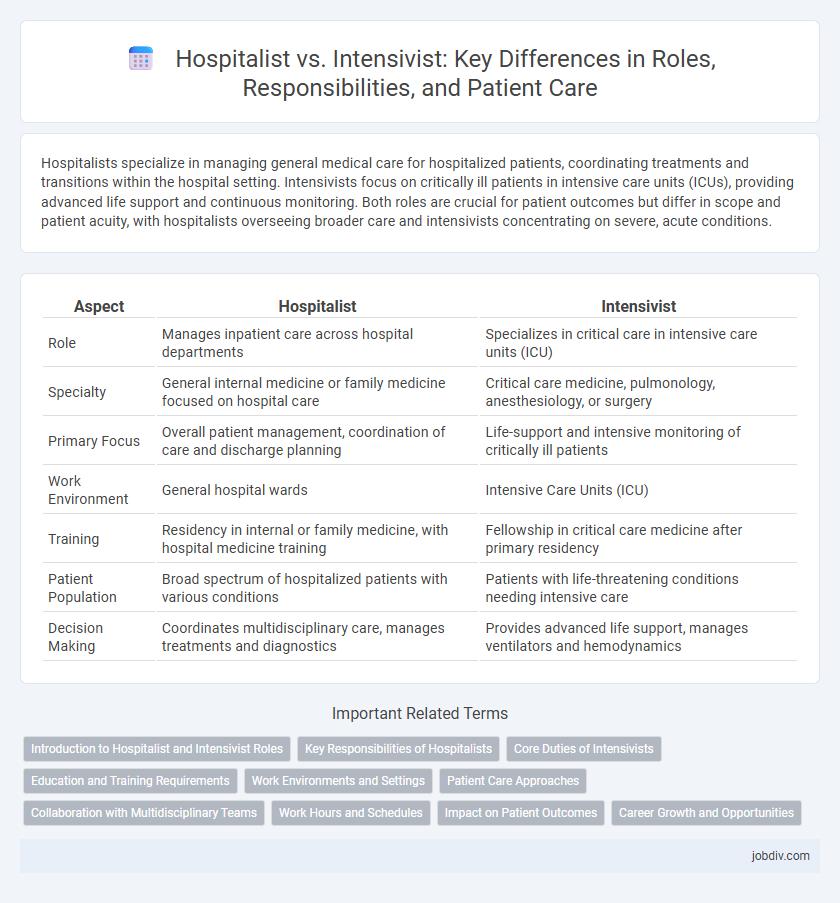
Hospitalists specialize in managing general medical care for hospitalized patients, coordinating treatments and transitions within the hospital setting. Intensivists focus on critically ill patients in intensive care units (ICUs), providing advanced life support and continuous monitoring. Both roles are crucial for patient outcomes but differ in scope and patient acuity, with hospitalists overseeing broader care and intensivists concentrating on severe, acute conditions.
Table of Comparison
| Aspect | Hospitalist | Intensivist |
|---|---|---|
| Role | Manages inpatient care across hospital departments | Specializes in critical care in intensive care units (ICU) |
| Specialty | General internal medicine or family medicine focused on hospital care | Critical care medicine, pulmonology, anesthesiology, or surgery |
| Primary Focus | Overall patient management, coordination of care and discharge planning | Life-support and intensive monitoring of critically ill patients |
| Work Environment | General hospital wards | Intensive Care Units (ICU) |
| Training | Residency in internal or family medicine, with hospital medicine training | Fellowship in critical care medicine after primary residency |
| Patient Population | Broad spectrum of hospitalized patients with various conditions | Patients with life-threatening conditions needing intensive care |
| Decision Making | Coordinates multidisciplinary care, manages treatments and diagnostics | Provides advanced life support, manages ventilators and hemodynamics |
Introduction to Hospitalist and Intensivist Roles
Hospitalists are physicians specializing in the comprehensive care and management of hospitalized patients, coordinating treatment plans and facilitating communication among various specialists. Intensivists, also known as critical care physicians, concentrate on the diagnosis and management of critically ill patients typically in intensive care units (ICUs), utilizing specialized skills in life support and complex interventions. Both roles play crucial parts in inpatient care, with hospitalists overseeing general hospital stays and intensivists addressing acute, life-threatening conditions.
Key Responsibilities of Hospitalists
Hospitalists coordinate comprehensive inpatient care, managing a range of medical conditions and facilitating communication between specialists, patients, and families. They oversee daily patient management, ensure timely diagnostic testing, and optimize treatment plans to promote recovery and prevent complications. Their role emphasizes continuity of care from admission through discharge, often collaborating with primary care providers for seamless transitions.
Core Duties of Intensivists
Intensivists specialize in the management of critically ill patients in intensive care units (ICUs), focusing on advanced life support, organ failure management, and complex decision-making for patients requiring mechanical ventilation or hemodynamic monitoring. Their core duties include coordinating multidisciplinary care, optimizing critical therapies, and implementing evidence-based protocols to improve patient outcomes during acute phases of severe illness. Intensivists play a pivotal role in invasive procedures such as central line placement, arterial catheterization, and advanced respiratory support, differentiating their practice from hospitalists who manage broader inpatient care.
Education and Training Requirements
Hospitalists typically complete a three-year internal medicine residency followed by board certification in hospital medicine, focusing on comprehensive inpatient care. Intensivists undergo additional fellowship training in critical care medicine, usually lasting one to two years after an internal medicine, anesthesiology, or surgery residency, to specialize in managing critically ill patients. Both roles require rigorous board certification to ensure expertise in their respective clinical environments.
Work Environments and Settings
Hospitalists primarily work in general hospital wards, managing a wide range of inpatient medical conditions, while intensivists specialize in critical care units such as Intensive Care Units (ICUs) where they treat patients with life-threatening illnesses or injuries. Hospitalists coordinate care across multiple departments, optimizing patient flow and discharge planning within structured, non-critical environments. Intensivists operate in high-stakes, technology-intensive settings that demand continuous monitoring and rapid intervention to stabilize critically ill patients.
Patient Care Approaches
Hospitalists focus on comprehensive inpatient care, managing a broad spectrum of conditions with continuous monitoring and coordination across specialties to ensure seamless transitions from admission to discharge. Intensivists specialize in critical care, providing advanced life support and monitoring in intensive care units, addressing acute, life-threatening conditions with high-tech interventions and rapid, precise decision-making. Both roles emphasize patient-centric care but differ in intensity and scope, with hospitalists overseeing overall hospitalization and intensivists managing complex, critical illnesses.
Collaboration with Multidisciplinary Teams
Hospitalists and intensivists collaborate closely with multidisciplinary teams to enhance patient care, especially in complex cases requiring intensive monitoring and treatment. Hospitalists coordinate general inpatient care and ensure seamless communication among specialists, nurses, and allied health professionals, while intensivists focus on managing critically ill patients in the ICU with input from respiratory therapists, pharmacists, and nutritionists. This collaborative approach improves patient outcomes, reduces hospital stay lengths, and supports comprehensive recovery plans.
Work Hours and Schedules
Hospitalists typically work structured shifts averaging 8 to 12 hours, providing continuous inpatient care during daytime hours with predictable schedules. Intensivists often engage in 12 to 24-hour shifts managing critically ill patients in intensive care units, requiring flexibility for overnight and on-call duties. The variability and intensity of intensivist schedules contrast with the more regimented, shift-based patterns common among hospitalists.
Impact on Patient Outcomes
Hospitalists improve patient outcomes by coordinating care during hospital stays with a broad focus on internal medicine, enhancing overall treatment efficiency and reducing readmission rates. Intensivists specialize in critical care for patients in intensive care units (ICUs), improving survival rates through advanced management of life-threatening conditions and continuous monitoring. Studies show that collaboration between hospitalists and intensivists leads to optimized care transitions and better recovery trajectories for critically ill patients.
Career Growth and Opportunities
Hospitalists primarily manage general inpatient care, offering diverse career growth through opportunities in hospital administration, quality improvement, and integrated healthcare systems. Intensivists specialize in critical care medicine, with career advancements often involving leadership roles in intensive care units, advanced procedural expertise, and research in acute patient management. Both career paths provide expanding opportunities driven by increasing demand for specialized inpatient and critical care services.
Hospitalist vs Intensivist Infographic
 jobdiv.com
jobdiv.com