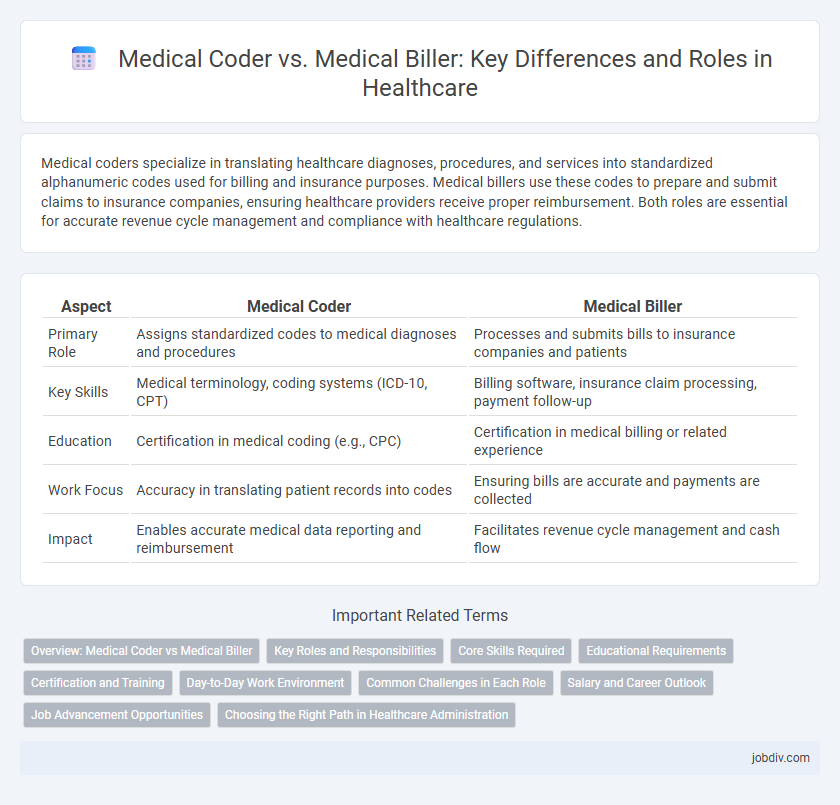
Medical coders specialize in translating healthcare diagnoses, procedures, and services into standardized alphanumeric codes used for billing and insurance purposes. Medical billers use these codes to prepare and submit claims to insurance companies, ensuring healthcare providers receive proper reimbursement. Both roles are essential for accurate revenue cycle management and compliance with healthcare regulations.
Table of Comparison
| Aspect | Medical Coder | Medical Biller |
|---|---|---|
| Primary Role | Assigns standardized codes to medical diagnoses and procedures | Processes and submits bills to insurance companies and patients |
| Key Skills | Medical terminology, coding systems (ICD-10, CPT) | Billing software, insurance claim processing, payment follow-up |
| Education | Certification in medical coding (e.g., CPC) | Certification in medical billing or related experience |
| Work Focus | Accuracy in translating patient records into codes | Ensuring bills are accurate and payments are collected |
| Impact | Enables accurate medical data reporting and reimbursement | Facilitates revenue cycle management and cash flow |
Overview: Medical Coder vs Medical Biller
Medical coders analyze patients' medical records and assign standardized codes for diagnoses, procedures, and treatments, ensuring accurate documentation for billing and insurance claims. Medical billers use these codes to generate invoices, submit claims to insurance companies, and follow up on payments, playing a crucial role in healthcare revenue cycles. Both positions require knowledge of medical terminology and healthcare regulations, but coders focus on data accuracy while billers handle financial processes.
Key Roles and Responsibilities
Medical coders specialize in translating healthcare diagnoses, procedures, and services into standardized alphanumeric codes essential for insurance claims and medical records. Medical billers manage patient billing information, prepare invoices, and submit claims to insurance companies to ensure accurate reimbursement for healthcare providers. Both roles require strong knowledge of medical terminology, coding systems like ICD-10 and CPT, and HIPAA compliance to ensure accurate and secure processing of healthcare information.
Core Skills Required
Medical coders require expertise in anatomy, physiology, medical terminology, and coding systems such as ICD-10 and CPT to accurately translate healthcare diagnoses and procedures into standardized codes. Medical billers focus on knowledge of billing software, insurance claim processes, payment posting, and understanding payer policies to ensure accurate and timely reimbursement. Both roles demand attention to detail, compliance with healthcare regulations like HIPAA, and effective communication skills to collaborate with providers and insurance companies.
Educational Requirements
Medical coders typically require a certificate or associate degree in medical coding or health information management, with coursework focused on anatomy, coding systems like ICD-10 and CPT, and healthcare regulations. Medical billers often pursue a diploma or certificate in medical billing, emphasizing insurance claims processing, billing software, and healthcare reimbursement methods. Both roles benefit from certifications such as Certified Professional Coder (CPC) for coders and Certified Medical Reimbursement Specialist (CMRS) for billers to enhance career prospects.
Certification and Training
Medical coders require certification such as the Certified Professional Coder (CPC) credential offered by the AAPC, which emphasizes mastery of ICD-10, CPT, and HCPCS coding systems. Medical billers often pursue the Certified Medical Reimbursement Specialist (CMRS) credential, highlighting expertise in billing processes, insurance claims, and payment posting. Both roles benefit from formal training programs, but coders focus intensely on coding accuracy and compliance, while billers prioritize billing software proficiency and claims management.
Day-to-Day Work Environment
Medical coders primarily analyze clinical statements and assign standardized codes for diagnoses and procedures, working closely with electronic health record systems to ensure accurate documentation. Medical billers focus on submitting claims to insurance companies and following up on unpaid bills, requiring frequent communication with healthcare providers and payers to resolve discrepancies. Both roles demand attention to detail and familiarity with healthcare regulations, but coders often work more independently while billers engage more directly with administrative workflows.
Common Challenges in Each Role
Medical coders often face challenges related to accurately interpreting complex medical documentation and ensuring correct code application for diagnoses and procedures, which directly impacts billing and compliance. Medical billers frequently encounter issues with claim denials, insurance follow-ups, and managing discrepancies in patient payment information that delay reimbursement. Both roles require meticulous attention to detail and up-to-date knowledge of coding standards such as ICD-10, CPT, and HCPCS to minimize errors and optimize revenue cycle management.
Salary and Career Outlook
Medical coders typically earn an average salary of $45,000 to $60,000 annually, while medical billers earn between $40,000 and $55,000, reflecting slightly lower compensation in billing due to differing responsibilities. Career outlook for medical coders is projected to grow by 8% through 2032, driven by increased demand for accurate health data management, whereas medical billing jobs are expected to grow at about 6%, influenced by healthcare industry expansion and billing system automation. Specialized certifications like Certified Professional Coder (CPC) can significantly boost salary and job prospects for coders, while Certified Billing and Coding Specialist (CBCS) credentials enhance opportunities for billers.
Job Advancement Opportunities
Medical coders often have opportunities to specialize in areas such as oncology or cardiology coding, which can lead to higher salaries and positions like coding supervisor or auditor. Medical billers can advance by gaining expertise in insurance claims processing and revenue cycle management, potentially progressing to billing manager or compliance officer roles. Both careers offer pathways to leadership positions within healthcare administration, emphasizing continuous certification and training for job advancement.
Choosing the Right Path in Healthcare Administration
Medical coders specialize in translating healthcare diagnoses, procedures, and services into standardized codes essential for accurate insurance claims and medical records. Medical billers focus on submitting claims to insurance companies, managing patient billing, and ensuring timely reimbursement for healthcare providers. Choosing the right path in healthcare administration depends on your detail orientation, interest in coding systems like ICD-10 and CPT, and preference for either data management or financial processes.
Medical Coder vs Medical Biller Infographic
 jobdiv.com
jobdiv.com